Meet our inspiring Runners-up of the VBHC Prize 2022
These initiatives will be shared with you here in rotation.
As healthcare professionals we have the responsibility to keep our society healthy. We should strive for healthcare without harm for our patients and planet.
The climate crisis is a health crisis. It leads to morbidity and mortality worldwide now. People are getting sick. Air pollution is all over, with effects on lung and cardiac disease. Rising temperatures are affecting the vulnerable. Heat associated illnesses are common. Infectious diseases are more globally spreading. Environments are changing in favour off for example mosquito’s and ticks. Mental effects are significant with anxiety, panic disorders and depression. We haven’t yet mentioned climate disaster like storms, flooding and fires which have a great impact on health and nature.
The healthcare sector in the Netherlands is responsible for approximately 7% of the total climate footprint. This number corresponds to our aviation sector. Our healthcare service is contributing to the climate change leading to an increased burden of disease.
We as healthcare providers should take our responsibility in reducing climate impact due to our service as much as possible. A sustainable approach in healthcare, also known as healthcare without harm, should be part of quality indicators.
To proceed to a sustainable way of working in our ED’s, we have founded the working committee GroenER (DSEP) last december 2021. The aim we have is to diminish climate impact by all Dutch Emergency Departments with 50% in next 5 years. We are going to reach this by creating awareness, sharing knowledge, connect local ED’s and stimulate a sustainable way of healthcare. To maximise impact we are working close together with the Dutch Urgent Aid Nurses Association. Because sustainable care should be the standard in healthcare we are also working multidisciplinary with other sustainable initiatives, like: ‘De Groene Zorg Alliantie’, ‘het Landelijk network de Groene OK’, ‘De Groene IC’ and many others.
We are building a platform to reach all above. This platform will be an online environment to connect and share and therefore stimulate and inspire each other. Besides that we are active in organising educational events. Our main coming event is a sustainable track live at the Dutch North Sea Emergency Medicine Conference. We will also present at the symposium Venticare Live which is a symposium intended for nurses working in acute care settings. Recently we have been presenting at the Amsterdam University (VUMC) talking about our sustainable journey we have started.
As Emergency Physicians we work with the ABC (Airway – Breathing – Circulation) structure and make sure we all speak the same language when treating our patients in the ED. For GroenER we have implemented an ABC structure as well, directly showing our adage: “Awareness and Best practice for Change, and don’t ever forget the Green Deal”.
Background
Today, shorter radiotherapy regimens are occasionally the option for treating early breast cancer patients for many countries12. However, newer treatment methods also implemented in Switzerland13 where breast cancer was the most common type of cancer for women, which caused around 1400 lives per year between 2008 and 2012.14 Traditional radiotherapy regimens with 25-fraction delivered over 5-6 weeks were widely used for many years as “standard course”, consisting of whole breast irradiation (WBI) after breast-conserving surgery (BCS) (e.g., 25×1.8 or 2.0 Gy) .1 Excellent survival allows alternating the radiotherapy paradigm undertaken for early and locally advanced breast cancer and improving long-term toxicity awareness and quality of life.2,3 The health care system must evaluate (quantify) newer treatment forms regarding their cost and effectiveness from the provider, payer, society perspective, and mutual understanding of its impact from the actual use. Thereby, physicians can create incentives to manage the treatment practices and ensure the quality of care rather than volumes. Time-driven activity-based costing (TDABC) as a bottom-up approach was defined as a suitable method estimating the hospital cost, including the direct fixed cost of equipment (price and maintenance) and direct variable cost of labor (salaries and benefits), well described by Kaplan and Anderson.
Purpose: A large amount of clinical evidence has been conducted to study the efficacy and safety of conventional 25-fraction radiotherapy regimens and compare them with a newer form of 5-fraction regimens for early breast cancer. The health care system must evaluate the health outcomes achieved per money spent. To investigate this, it is performed cost-effectiveness analysis for two treatment strategies comparing costs with clinical outcomes.
Materials and methods: A literature search is conducted from the RCTs study that evaluated clinical outcomes of 25-fraction and compared to 5-fraction regimens. Treatment plans data are extracted from ARIA software, also observations and consultations with staff members. Time-driven activity-based costing (TDABC) is used to estimate the hospital costs and
included the direct fixed cost of radiotherapy (equipment) and direct variable cost (personnel). The TARMED tariff was used to calculate tax points collected from each service provided to patients and converted to money values. The societal cost was defined as productivity loss (e.g., absence from work) according to the Swiss Household panel data (SHP) from 2018.
Results: The study found that 5-fraction regimens resulted in a total of 62% cost reduction for hospital, 51% insurance and 93% society. The RCTs examined the clinical outcomes and showed that 5-fraction regimens are not significantly different for normal tissue effect (NTE) and tumor recurrence compared with 25-fraction regimens according to their predefined objectives.
Conclusion: 5-fraction radiotherapy regimens are estimated to be less costly than conventional 25-fraction regimens. More studies should be conducted to define the optimal treatment strategy and willingness to pay for the health outcome achieved.
Possible real-life impact: In recent years, healthcare is developing, and expenditure constantly increases in Switzerland, reaching around 12% of the gross domestic product (GDP), making it one of the world’s priciest healthcare systems after only the United States (US). The system’s transition requires a detailed understanding of healthcare costs encompassing transparent reporting of outcomes upon individual assumptions. These findings may help policy makers and physicians formulate cost-effective radiotherapy evidence-based practice and meet patients’ needs.
The obesity surgical treatment integrated responsability centre (CRI-TCO) is a clinical pathway treatment developed in the Central Lisbon University Hospital Centre from Portugal. In the CRI-TCO the patients have a fully integrated treatment for their obesity, using the best available evidence in their treatment.
We have a differentiated clinical support structure that prepares and guides the obese patients in their care path, which allows them to achieve more efficient results, with financially sustainable costs for the SNS. The action of this initiative is centered on clinical protocols, based on scientific evidences, promoting the integration of care in a patient holistic perspective and provides also the opportunity of sharing knowledge between all professionals.
It has a patient experience group which meets on a quarterly basis to collect advice and strategic guidance with the aim of developing high-quality, patient-centered care.
In our approach we have an intervention from 10 different specialties using a hybrid consultation approach, both with teleconsultations and in a presential basis. This is done in our obesity treatment clinic, were we have a nurse case manager that evaluates the quality of life of patients in all the treatment process.
The case manager methodology was implemented as a collaborative process in which the “Case Manager Nurse” monitors the patient’s health situation, promotes an effective evaluation and diagnostic assessment in order to ensure an efficient multidisciplinary care path to each patient/user. Is this case manager that evaluates the quality of life of the patients along the pathway allowing to understand the health outcomes of this program.
The surgical team has a high quality of care and expertise in most accurate and successful laparoscopic bariatric techniques including robotic approach, with fewer surgical complications and an increasing reduction on hospital stay (average 2 days). We are the only Hospital in Portugal that uses the robotic surgery to this treatment and we are at this time evaluating the costs and effects for patients.
After surgery, patients are followed up through telefone/presencial nursing consultations at 48, 72h post-surgery, also at third and sixth month, second and third year in order to ensure the continuity and safety of team care.
1.1 Introduction
The prevalence of obesity and overweight among children is high in Aruba. UNICEF reported that
obesity is the biggest public health problem affecting children and adolescents in Aruba (UNICEF,
2013). Among preschoolers 25,6% of girls and 17,8% of boys were overweight or obese in 2010. This
number was bigger among fifth graders in primary school where 43% of girls and 32,4% of boys
were overweight or obese (Ministry of Public Health and Sport, 2013). According to the World Health
Organization, children who are overweight tend to stay overweight as adults. Furthermore,
childhood obesity is associated with noncommunicable diseases in adulthood such as cardiovascular
disease, type 2 diabetes mellitus and psychosocial (Weihrauch-Blüher & Wiegand, 2018) which
further contributes to the rising costs of healthcare (Pan American Conference on Obesity, 2011).
Various efforts are already in place to tackle childhood obesity in Aruba. These include the call to
action plan in 2011 (https://www.paho.org/en/documents/aruba-declaration-call-concerted-actionobesity-
special-attention-childhood-obesity) and the creation of an institute for healthy and active
living (http://ibisa.org.aw). However, based on different patient encounters with overweight
children at the ambulatory pediatric department of the Horacio Oduber Hospital, Aruba, we
identified that there was a need for concerted and more focused efforts to address this problem.
Some of these efforts include educating children and their parents about healthy lifestyles and how to
achieve this through physical activity and dietary modification.
Therefore, this project was set up to provide answers to these needs by using a multifaceted
approach based on four strategic pillars; 1) physical activity, 2) education and 3) nutrition supported
by the last pillar, 4) research.
1.2 Objectives
The aim of the JUMP18 project is to set up a long-term plan to treat and prevent childhood obesity in
Aruba. We intend to achieve this through focusing on four pillars for change namely:
1. Education
2. Nutrition
3. Physical activity
4. Research
1.3 Mission
Our mission is to ensure the healthy well-being of Aruban children by reducing the burden of disease
associated with childhood obesity. Through the JUMP18 project, we created opportunities for Dutch
Caribbean students and health care professionals to contribute and improve the health of children in
Aruba. With the combined knowledge and collaboration of various health care disciplines, we plan to
reduce childhood obesity in Aruba significantly both in the short and long term.
1.4 Vision
To eradicate the incidence of childhood obesity in Aruba and improve the overall well-being of
Aruban children. By 2022, the incidence of childhood obesity in Aruba will be reduced by 20%, 50%
in three years (2025) and by 80% childhood obesity in five years.
- Why is Quality of Life so important in the diagnosis and treatment of Myeloproliferative Neoplasm Blood Cancers? Blood counts and their associated numbers only tell one side of the patient story. The other side of the story is one’s quality of life. How is the patient living with this condition? How are they coping with the day to day demands of life and how is their MPN condition affecting this?
- Quality of life data from patients has never been tracked or has never been added to the dialogue between patient and physician. The longitudinal quantification of Q of L symptoms of this disease can provide clues to both patients and physicians as to their daily struggles and this can lead to the consideration of medical or non-medical interventions and perhaps even to foresee progression of the disease. We can even see a future where Q of L data can be correlated to disease progression and further assist patients and physicians with care decisions. This data will improve the care of MPN Patients.
- While the long-term objective of this project is really the improved care of MPN patients, the road to this end goal is really arrived at by the added sum of other goals. These near-term objectives of this project are
- to set up a Quality-of-Life data collection system making use of phone/tablet App technology
- to set up a Real-World Evidence of Quality-of-Life data sharing network available to all stakeholders
- to set up a Quality-of-Life Data bank
- Once these goals are achieved and the ecosystem is in place, we believe this can be used to accomplish shared treatment decision making that will contribute to the overall diagnosis and treatment of a patient’s mpn blood cancer. It will maximize efficiency and effectiveness of the clinical visit of the mpn patient and their Hematology Physician through the sharing of patient data on their quality-of-life symptoms with an MPN Blood Cancer and to encourage Shared Treatment Decision Making.
Thanks to the support of the A.A.E.E. – APS Patient Association, the patient’s current unmet needs were identified. In a structured way and with the participation of Clinicians, Hospital Pharmacists and Pharmacoeconomists, the four phases of management of the patient with HAE were examined: diagnosis, pharmacological treatment, acute episodes, monitoring and follow up. The AS IS process was mapped on these and the current criticalities identified.
From the analysis of the AS IS processes and the identification of criticalities, a TO BE model was developed, according to a LEAN management approach, which, if implemented, would help to have a more rapid diagnosis and a better taking charge and management of the patient affected by HAE, both for the patient and for the social and health system as a whole.
When the Model is applied to the patient journey of the patient with HAE in its 4 primary management phases (diagnosis, treatment, acute episodes, monitoring and follow up) it can bring significant advantages both to the patient and to the health and social system as a whole.
If it’s applied to the diagnosis phase, it determines for the patient the possibility of being treated early and with the right therapy, allowing the health and social system to save direct and indirect costs.
If it’s applied to the pharmacological treatment phase, it determines for the patient the availability of drugs when necessary, and in the necessary quantity and for the social and health system, the possibility that hospital and local pharmacists procure drugs in a more fluid and programmed way, also reducing waste.
If applied to the management phase of acute episodes of the pathology, it determines for the patient the possibility of receiving treatment promptly in the acute phase, and for the health and social system it involves lower direct and indirect costs (waste related to access to the emergency room would be avoided)
Finally, if the LEAN model is applied to the management phase of the monitoring and follow-up of the patient with HAE, it determines for the patient the possibility of being able to be treated adequately over time and in the event of evolution of the pathology, accessing the most suitable drugs based on his conditions. updates and the advancement of clinical research. It seems desirable that the LEAN model be implemented and implemented on the national scene, in a dual propositional key: to ensure proper care and management of the patient suffering from a rare disease and to avoid waste of health care costs.
Epilepsy Foundation India is a Mumbai based organization working to provide comprehensive epilepsy care and rehabilitation of persons living with epilepsy in rural areas of Maharashtra. Soon after its inception in 2011, the Epilepsy Foundation of India started working with the National Health Mission, Govt. of Maharashtra, MoHFW (India). The organization has served more than 45,000 providing diagnostic, free treatment & follow up services, therapy, employment and marriage assistance, yoga classes, etc. This was being done via organizing field medical camps with a team of medical experts and devices at rural district hospital locations in India. Besides rural services Epilepsy Foundation India runs free OPD in Mumbai for past 22years and provide free medication besides other services.
The impact of sudden cessation of consultations and access to medicines post the pandemic lockdown since March’2020 has been hugely felt in this vulnerable section of the Indian population. Due to the covid lockdown following challenges were faced by Health care and patients
1. OPD services as well as Epilepsy Camps were closed
2. Medicine availability was compromised
3. Loss of job and income sources, reduced the capability of medicine purchasing
4. Because of COVID restrictions, regular consultations were closed
Integrated Practice Unit (IPU) of epilepsy care experts delivered technology-aided long-term care to patients in rural Maharashtra at home with complete access to specialists and at zero cost to patients. This was done in collaboration with the National Health mission, Govt. of Maharashtra who audit the activity and provide financial assistance for the initiative.
The Integrated Practice Unit providing the care consists of a team of neurologists, neurosurgeons, psychologists, physiotherapists, occupational therapists, speech therapists, technicians, social worker & care giver etc. work together to provide quality epilepsy care in Urban as well as Rural India to the PWE.
The IPV also included PWE (Person with Epilepsy) with their skill to do advocacy & serve other PWE. (like tuition, yoga training, craft classes etc.)
Since 2013 Takeda is a partner of the National Health System to enhance and disseminate the benefits of Lean management in the healthcare by creating a Value Based Partnership entirely dedicated to the benefit of patients.
Over the years, Takeda has expanded his commitment to spreading this management system – born in Japan in the 1960s – and its application in the healthcare sector, supporting various programs that are still in progress.
Takeda believes in the value of this approach, especially in a historical phase characterized by limited resources and, at the same time, by the availability of important new therapeutic options and technologies that must be made accessible for all patients.
The commitment today is to support the awareness of a Lean culture in healthcare so that this approach is not confined to a few virtuous experiences but can become a system approach.
It will thus be possible to abandon the concept of Lean Management in Healthcare in favor of Lean Management for patients.
The continuous reduction of waste and the increase of value in patient pathways, embraced by the Lean Methodology, is used as an enabler to shift to Value Based Healthcare, by putting the patient at the center of the analysis and increasing the outcomes related to the pathway. Other Lean concepts like the need to overcome functional structures and work in a multidisciplinary approach, the need to describe performances and results with specific measurable KPIs, the focus on patient value, all perfectly match the requirements of VBHC.
Over the years, Takeda has created numerous partnerships with Regions or Hospitals to improve patient care pathways through Lean projects, applied the methodology internally with projects and training and sponsored Master of Science hosted by Universities and Hospitals and sponsored the main Lean Healthcare initiatives in Italy. Amongst the initiatives, one to highlight is the “Lean Healthcare Award ” a competition born in 2018 with the aim of rewarding the best reorganization and innovation projects in the Healthcare world in Italy, which in the years stood between the others as the go-to choice for Lean-savvy organizations to show their improvement projects.
The research project hereby described aims at analysing current clinical practices used in the management of multiple myeloma patients and identifying an optimal model based on lean management techniques. The study involves major clinical centres in Italy identified according to the number of cases treated annually. After the analysis of the literature, aiming at understanding current practices worldwide, we presented the project to the top management of the clinical centre involved. To analyse actual way of working we will conduct a focus group administering a questionnaire developed based on guidelines, literature review and on the critical point regarding the management of this pathology. Now we are currently finishing this stage of the project. The next point will include the cost analysis of the entire pathways through the economic enhancement of each step. This project is particularly relevant due to the incidence of the pathology and the innovativeness that regards some techniques that have been recently introduced. Furthermore, through the identification of the optimal model we aim to improve the overall satisfaction of the patients, positively impacting the health system sustainability, giving value to the professionals involved.
The Electrophysiology (EP) Learning Network is made up of 51 cardiac electrophysiologists from 28 United States organizations. One of the primary goals of the network is to build the infrastructure to embed outcomes collection into EP workflows which is a necessary foundational characteristic to create value-based payment models. We are achieving this by sponsoring patient outcomes data collection initiatives funded by industry grants. Through these grants we create the building blocks for institutions to collect outcomes data, build QI capacity and engage in physician-driven research collaborations.
Improving quality and accountability depends on having a shared goal that unites the interests and activities of all stakeholders.1 Through this learning network, we are prompting a culture of collaboration, transparency and quality. Participating institutions use our solutions to collect patient, procedural and long-term outcomes data for patients undergoing atrial fibrillation ablation procedures – which are used to restore the normal heart rhythm.
Our focus on physician-driven collaboration ensures that providers of care are aligned on our mission and goals. The next step will be to facilitate collaboration amongst all stakeholders in the care continuum of atrial fibrillation. While we have started with physicians, we are committed to engaging patients. It is our mission to promote shared decision making where physicians know their outcomes and can communicate them to their patients, and patients have access to their physician’s outcomes, quality, safety and effectiveness.
We began with physician collaboration because there is still significant heterogeneity in care delivery for atrial fibrillation (AF). Our network is working to develop and achieve consensus around the optimal care model as an important first step in advancing VBHC in AF. Consensus and evidence around the delivery system is necessary before alternative payment models can be developed and tested.2
Within the network, we systematically collect data on how participation influences practice. We collect data on how and what practices have changed. We also assess attitudes towards outcomes transparency, psychological safety and burn-out. Physicians have reported that participation in the network and registry-related data collection has helped with their burn out and overall job satisfaction. We are building a system to support transparency of outcomes and collaboration with peers, patients, and the public.
Through this platform, we are giving many institutions who previously did not have the capacity or experience in collecting outcomes the opportunity to know, learn from and be transparent with their patients about their own outcomes. It provides them the opportunity to participate in research and nationwide quality improvement efforts. The initiative also gives patients in these communities access to opportunities for research participation and care from clinicians that are quality-focused and data driven, which improves diversity and representation of patients in evidence-generation.
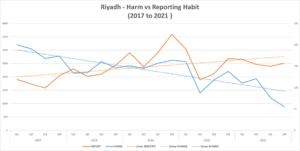
The life of every patient, family, staff and volunteer at King Faisal Specialist Hospital and Research Centre is precious and there is no greater responsibility than keeping them safe from harm. While we perform above international benchmarks for safety, we believe the only acceptable standard for harm is zero. On 1 November 2017 KFSH&RC committed to a goal of zero harm to not only strengthen our leadership role and reputation but set a new standard of excellence.
Medical error is the third leading cause of death in USA, and a major cause of waste in healthcare. It is estimated that about 20 to 30% of healthcare expenditure is waste. Despite efforts to reduce errors and waste, the number of deaths because of medical errors is increasing since 2000 (IMO report, to Err is Human). As of a recent study published in the BMJ in 2016, it is estimated that the number of deaths reached 251,454 based on the number of admissions in 2013 to USA hospitals.
The Aim of the journey is to eliminate preventable medical mistakes, which we have names as “Zero Harm”
The size and scope of this journey is organization wide across two hospital locations (located in Riyadh and Jeddah). KFSH&RC is a Multi-Accredited Tertiary/ quaternary specialised academic hospital, The Riyadh location has 1,100+ beds, while Jeddah is a 350+ bed hospital.
With our partnership with International consulting body “Press Ganey –HPI” group, the methodology taken was based on high reliability science, utilized in several premier hospitals in US and Canada; such as Mayo clinic. The methods include but not limited to:
- Establishment of a multi-tiered huddle system (from front line to executive)
- Enculturation of universal error-prevention behaviours skills
- Just Culture adoption
- Robust process improvement and Patient Safety methodologies
Over the course of the past few years, our average harm rate (which encompasses infections, sentinel event, never events, serious safety events, etc.) has dropped, which an increase in reporting habit of the organization.
Becoming a high reliability organization (HRO) and achieving zero harm is not a project. It is not a program, it is a journey.
The “Digital Health Project 4.0” is one of the main technological innovation projects being
implemented and ongoing at Sao Paulo University Medical Scholl Clinics Hospital, Hcfmusp (*).
We are one of the largest hospital complexes in South America, serving as a teaching hospital for
the Medical School. The hospital complex operates on four fundamental pillars: Assistance,
Education, Research and Innovation. Medical School started in 1912 and the associated teaching
hospital starded activities in 1944. Located at the city of Sao Paulo, the hospital complex has 2,500
beds; 450 ICU ; 10 ten Institutes; 20,000 professionals, including medical, nursing, administrative
and students; 2 chronic diseases hospitals; 62 medical research laboratories (biochemistry,
molecular biology, medical informatics, internal medicine, etc.). Assistance: More than 1.5 million
outpatient consultations per year; More than 76,000 hospitalizations per year. Education: More than
2,000 resident physicians per year. Innovation: InovaHC, our innovation hub, has 14 solutions and
3 major programs to accelerate innovation in healthcare. Project objectives: develop scalable digital
health solutions at the national level, based on lessons learned in the design of the digital health
strategy at the largest hospital complex in Latin America. Vision: Hcfmusp aspires “To be a
protagonist in innovation in Digital Health at all levels of care with excellence in care, teaching and
research, aiming to improve the quality, access and equity of the system”. Pillars: the strategy will
focus on (i) improving the patient experience; (ii) increase the capacity of the health network; (iii)
create innovative solutions, including Primary Care and digital health workforce preparation. Goals:
Hcfmusp has committed to 10 concrete and measurable goals by 2023, such as a 40% reduction in
face-to-face consultations and 30,000 patients assisted by remote telemonitoring. We observed that
a new strategy was necessary in order to coordinate all different initiatives running at our 10
institutes. A multidisciplinary team (clinical, administrative and instructors) from all institutes
detailed 20 twenty initiatives to realize the ambition of the strategy in patient care, education,
research and primary care. The 20 initiatives are: 1 Teleconsultation; 2 Digitization of the Patient’s
Journey; 3 Virtual Visit of Relatives to Inpatients; 4. Telerehabilitation; 5. Electronic Medical
Record Interoperability; 6. Use of Virtual Reality; 7. Patient Experience Unit; 8. Second opinion
tele interconsultation; 9 . Teleconsulting; 10. Remote operation of hospital equipment; 11. Urgency
and Emergency Teleregulation; 12. Use of Artificial Intelligence for the interpretation of
Radiological Images; 13. Use of Artificial Intelligence to support the indication of exams; 14.
Training and Qualification in ICU; 15. Surgical Teletraining: Remote Teaching of Surgery; 16.
Digital Primary Care Pilot; 17. Remote telemonitoring of patients; 18. Service Platform for the SUS
network (Brazilian Public Health System); 19. Telemedicine; 20. Continuing Education in Health.
The project is carried out within the Better Healthcare Program (BHP) initiative (**), which is a
cooperation program between the UK Government and the Brazilian Ministry of Health, with the
support of McKinsey&Company (www.mckinsey.com.br/) (***) as a management and consulting
support. We have started intensive use of digital health tools and technologies, such as
Telemedicine, Artificial Intelligence, Machine Learning, Telemonitoring, among others during the
pandemic in 2020-2021. The new stategy of alignment using a value-based heathcare model proved
to be essential. RESULTS: We have advanced significantly patient´s teleconsulting andtelemedicine online assistance.
Our goal is to achieve 40% of outpatient care online by 2023.
PATIENTS: lower costs and better outcomes; PROVIDERS: higher patient satisfaction rates and
better care efficiencies; PAYERS: stronger cost controls and reduced risks; SUPPIERS: alignment
of proces with patient outcomes; SOCIETY: reduced healthcare spending and better overall health.
In addition to improving patient care in the hospital itself, we sought to leverage its vocation for
education, research and public policy to assume a pioneering role in promoting digital health
solutions at all levels of care on a national scale.
(*) https://www.hc.fm.usp.br/
(**) https://www.gov.uk/government/publications/better-health-programme
(***)https://www.mckinsey.com.br/