JOINT VALUE; an integrated network creating, in collaboration with patients, value over the full patient journey of Inflammatory arthritis. This (digital) network connects patients, primary-care and hospitals by implementing Porter’s VBHC-strategy and is unique because of its scientific approach to gather evidence for its added value.
Inflammatory arthritis (IA) is a common joint disease that, when not treated in an early phase, results in progressive loss of physical, psychological and social functioning. Approximately 100 to 300 of the 1000 adults have lifelong IA. IA is a ‘high-value burden’ disease due to life-long treatment with biologicals (Netherlands 0.74% of healthcare cost), high comorbidity (67% of IA patients) and low work-participation (20–70% work-disabled). Timely intervention and outcome-based monitoring decreases the burden of disease. Timely means early recognition in primary care. Reality is that IA is hard to recognize by general practitioners (GP) leading to diagnostic delays up to 8-10 years and inefficient referrals up to 80% to costly secondary care. In daily practice outcome-based monitoring focus on biomedical outcome, is fragmented over the full care cycle and not benchmarked between caregivers.
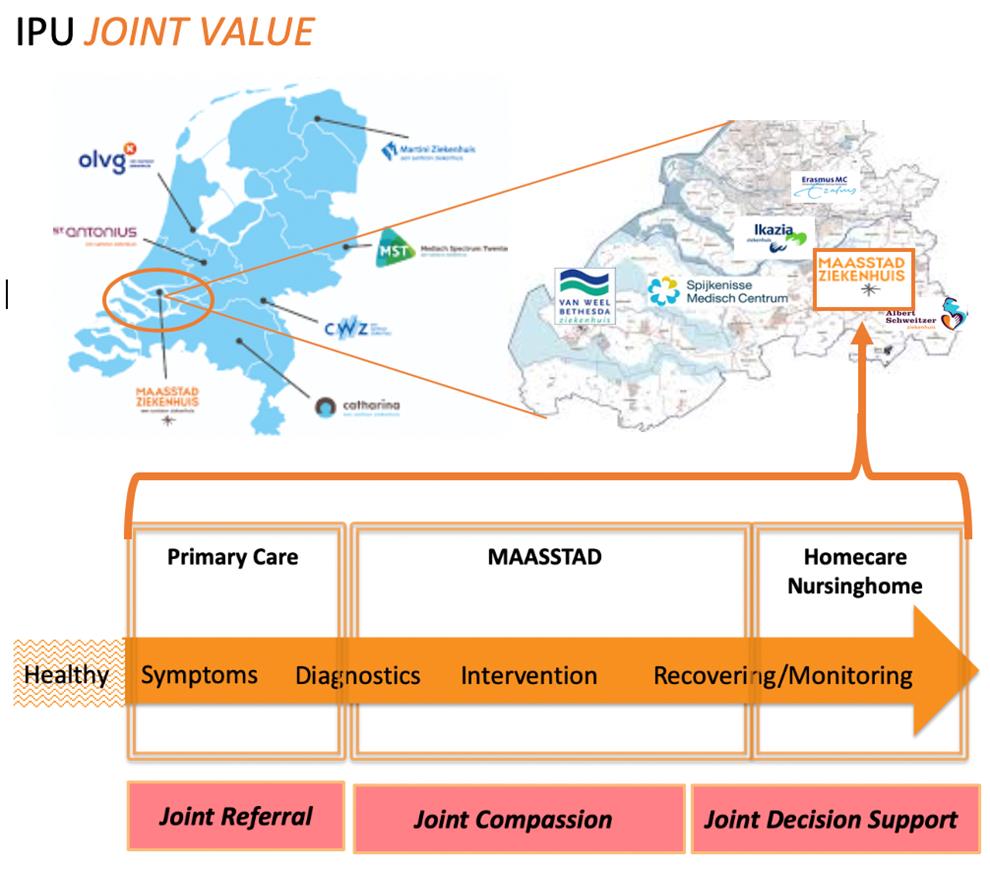
JOINT VALUE conducted 3 main programs: Joint referral > Joint Compassion > Joint Decision Support;
Joint referral, an integrated care network of regional hospitals and primary carecenters, facilitates timely cost-effective referrals. Since the start in 2010 access time is continuously below the (inter)national standard of 4 weeks, whereas this is 4-28 weeks in the Netherlands. In 2018 our innovative digital algorithm that supports GPs was implemented and showed a 40% reduction in referrals while patient outcome (PRO) did not decline. A significant cost-effectiveness effect was seen (ICER €17.000). In 2019 triage by a rheumatologist in a primary care started and showed 70-80% referral reduction.
Joint compassion started monitoring on relevant outcomes on the patient and organization level. After participating in the ICHOM IA workinggroup we implemented the ICHOM IA standardset for goal-based shared decision-making. Preliminary results (n=600) indicate that what patients matter the most, differs from the outcome recommended by international guidelines and based on these results different journeys were made for multimorbid IA patients. Benchmarking outcomes started in 2018 by the Santeon collaboration, seven hospitals (11% of the Dutchcare) work together with the aim of adding value by continuous evaluation of outcome and cost. This Santeon collaboration resulted in transparency and improvement of outcomes and a 70% reduction in medical cost (biologicals).
Joint decision support gives digital support for patients and caregivers during the lifelong monitoring phase. An innovative dashboard showing ICHOM outcomes (honored by Dutch NHI), built in 2019 in close collaboration with patients, enables shared decision making, remote patient home-monitoring and coaching (self-management) to ultimately prevent progression of patient outcomes and re-hospitalization.
Upscaling to other regions is very realistic as this program fits in the Dutch healthcare system and contributes to the national strategy of right care at the right place. Upscaling the digital support systems to other indications and organizations is realistic since it is based on reliable and secure cloud platform with FAIR principles.